Healthcare System in the Central Okanagan
COEDC News June 18, 2025

A reliable healthcare system is the foundation of a thriving community. For the Central Okanagan, ensuring that residents have access to timely, quality care is not just a public health priority, it’s an economic one. That’s why the Central Okanagan Economic Development Commission (COEDC) dedicated its Advisory Committee meeting in May to a critical and timely issue: the recruitment and retention of physicians in our region. The COEDC Advisory Committee is a 45-member group made up of industry leaders, community shapers and elected officials. The Committee meets monthly to share information and work together towards sustainable economic growth.
This meeting brought together key voices from across the healthcare landscape, including representatives from Doctors of BC, the Central Okanagan Division of Family Practice (CODoFP), and the Interior Physician Recruitment & Retention Network (IPRR). Their insights painted a clear picture of the challenges the region faces and the opportunities available to us to make a difference.
Why This Matters to the COEDC
The COEDC’s mission is to foster a resilient and prosperous economy in the Central Okanagan. But economic growth is only sustainable when people feel safe, supported, and healthy. A strong healthcare system is essential for attracting and retaining talent, supporting families, and ensuring that businesses can thrive.
When doctors leave a region, it’s often not because of the job itself but because their families haven’t found a sense of belonging. Due to this they often prefer moving to larger urban centers. That’s where the COEDC can play a transformative role: by supporting connections for Doctor’s partners and families to find high level employment and create roots in the community through programs like Connector and the Okanagan Young Professionals Collective. The Connector Program is a simple, effective, no-cost referral process that links newcomers with well-connected individuals to better integrate into the workforce and settle successfully in the region. Meanwhile, the OYP Collective hosts monthly coffee socials to expand their social and professional networks in the community.
A Closer Look at the Presentations
Dr. Laurie Main and Brent Weiss from Doctors of BC opened the discussion with an overview of their organization’s mission. Formerly known as the BC Medical Association, Doctors of BC is focused on empowering physicians to lead improvements in the healthcare system and patient care. Their work is grounded in collaboration between doctors, communities, and policymakers.
Beth Whalley, Executive Director of the CODoFP, and Dr. Milt Stevenson of the IPRR, shared how their organizations are tackling the physician shortage head-on. The IPRR was formed to address retirement among local doctors. Their approach begins at the community level, gathering data and insights, and then advocating at the provincial level for the resources and policy changes needed to support recruitment and retention. The CODoFP supports local family doctors and works to improve access to quality primary health care for patients in the Central Okanagan region.
The Challenges Faced
The conversation quickly turned to the real-world challenges that are making it difficult to recruit and retain doctors in the Central Okanagan.
One of the most pressing concerns is workplace safety. One in three doctors has experienced violence on the job, yet there is no formal psychological safety training or reporting mechanism for hospitalists or independent contractors. A healthy workplace culture is essential not just for retention, but for the well-being of those who care for us.
The administrative burden on physicians is another major issue. Under the new Local Family Physician (LFP) payment model, doctors can spend more time on complex cases providing better care than with the former fee for service model. However, this model doesn’t provide funding for hiring assistants or managing the significant administrative workload. For every hour spent with a patient, doctors often spend more than an hour on follow-up paperwork. AI tools aren’t yet reliable enough to help in a meaningful way, and most physicians receive no business training to manage these demands.
Access to care is also uneven. While new health hubs for traditional ongoing healthcare are helping some patients, they tend to serve middle-class individuals who already have a family doctor. Many others, especially vulnerable populations, are falling through the cracks and are not being served in those settings. More community-based clinics with navigators and group resources are needed to ensure that everyone can access care and avoid unnecessary emergency room visits.
Barriers to Recruitment
Recruiting new doctors is a complex process, especially for International Medical Graduates (IMGs), many of whom are Canadian citizens. The cost and time required to get certified and practice in BC are staggering. A two-year UBC residency for an IMG costs taxpayers $500,000, compared to just $130,000 for a 12-week Practice Ready Assessment for graduates from other countries. Doctors from the UK, Ireland, the US, and Australia don’t come with additional costs.
Even once recruited, doctors face bureaucratic hurdles. The paperwork required to practice in BC is extensive, and contracts for specialists must come from Health Authorities rather than recruiters, creating delays and confusion. The IPRR is actively working to streamline the process for physicians from other jurisdictions to begin practicing in the region and to accelerate interprovincial registration.
Retention: More Than Just a Job
Retention is about more than just the work; it’s about the community. Many exit surveys reveal that doctors leave because their families haven’t found a connection to the community. This is where the COEDC can make a real impact by helping the partners and families of doctors access professional networks in their respective fields through the Connector program.
The need for specialists is also growing. While some areas of the province have been working on specialist recruitment, the Central Okanagan has been limited by funding and the inability to offer contracts they don’t own. This has created a disconnect that must be addressed if we want to build a collaborative, comprehensive care model.
A System Under Strain
Maternity, pediatrics, and long-term care are in crisis due to administrative burdens, scheduling challenges, and on-call demands. The CODoFP is specifically funded to ensure that individuals moving into long-term care facilities maintain a family physician, but the system is stretched thin.
The unattachment rate, people without a family doctor, is estimated at 30–40% of the population. The good news is that 12,000 people were matched with a GP last year. Unfortunately, 14,000 remain on the waitlist and many others are likely unaware of the registry. The attachment team at the CODoFP plays a vital role in building the human relationships that make care possible.
Innovative Solutions and Community Support
Innovation is happening. The Physician Waffle House, an online platform developed in Vernon with support from an ETSI-BC economic development grant, offers peer support, leadership training, and help finding locums for when a doctor is away. It’s a promising model for how technology and community can come together to support doctors.
The Primary Care Network is also evolving. Its virtual nature allows for flexibility in how care is delivered, opening the door to new models of service that can better meet the needs of diverse populations.
Taking Action: A Community-Wide Effort
Addressing the healthcare challenges in the Central Okanagan requires a united effort—and there are tangible ways we can all contribute.
First, by raising awareness and sharing valuable public resources like the Central Okanagan Primary Care Network and the Health Connect Registry, we can connect residents with the care they need and reduce pressure on emergency services.
Second, we can support physician retention by helping new doctors and their families feel welcomed and integrated into the community. Whether it’s through employment opportunities for spouses or social connections.
Finally, advocacy efforts can focus on streamlining processes to allow doctors from other jurisdictions to practice here more easily and ensuring healthcare professionals receive the support they need to thrive.
Healthcare and Economic Development: Inseparable Priorities
A strong healthcare system isn’t just important for people, it’s also important for businesses looking to recruit and retain their workforce. Families are more likely to stay in the region when they feel secure. And professionals are more inclined to relocate to communities where they know quality care is accessible.
The COEDC is committed to being part of the solution. By working together across sectors such as healthcare, business, government, and community, we can build a system that supports doctors, serves patients, and strengthens our economy.
You Might Also Like...
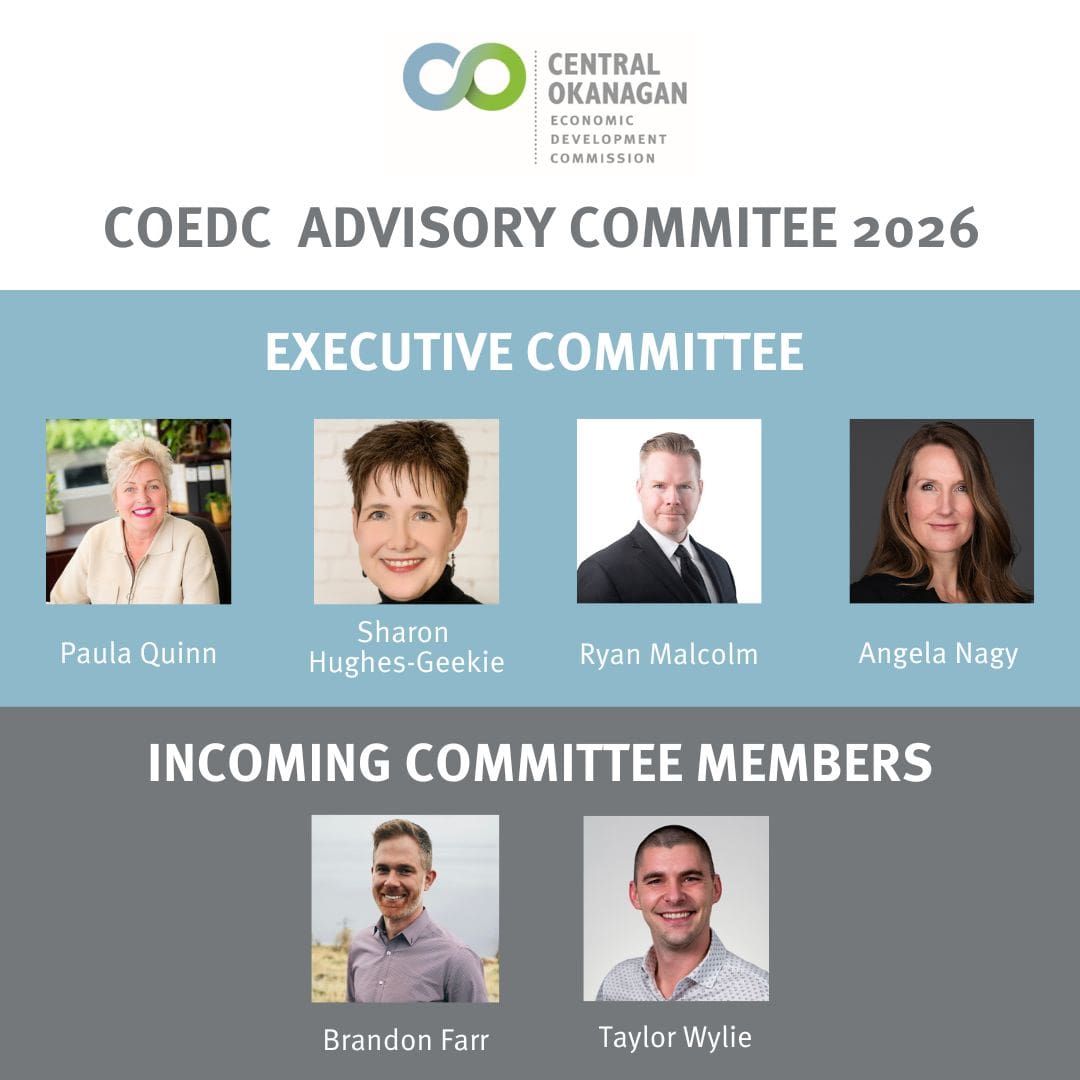
COEDC announces 2026 Advisory Committee members
The committee convenes monthly to exchange information and works to foster sustainable economic growth in…
Advisory Committee January 30, 2026
Okanagan Manufacturing Network launches to unite and strengthen local manufacturers
New association connects, supports and celebrates the makers powering the Okanagan economy
COEDC News January 16, 2026
Kelowna Recognized as UNESCO’s City of Gastronomy
November 26th, 2025 Advisory Committee Recap
Advisory Committee December 4, 2025